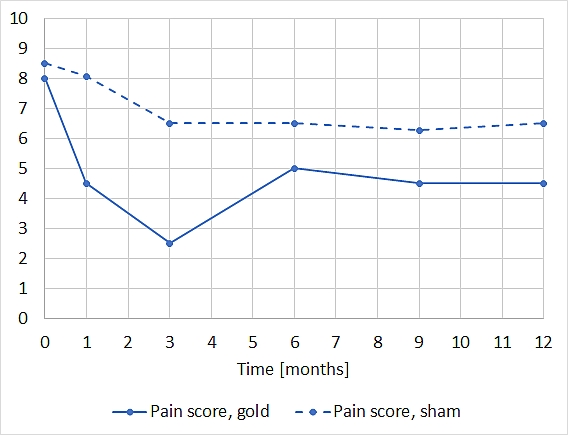
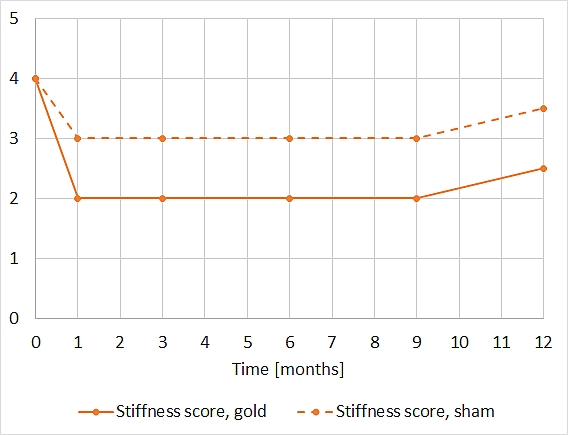
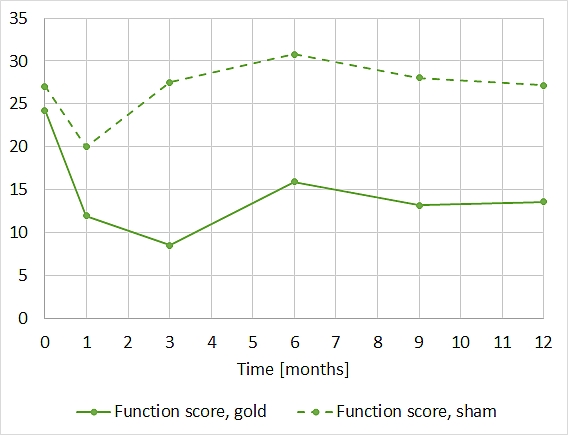
Randomised controlled trial of extraarticular gold bead implantation for treatment of knee osteoarthritis: a pilot studyBesides pharmacological and surgical treatment of knee osteoarthritis (OA), acupuncture represents a further recognised effective alternative, although the improvement is often short-lived and the acupuncture thus has to be repeated regularly. Gold implantation at the acupuncture points, which has been used in dogs for at least 30 years and has demonstrated an effect for several years, is hypothesized by the authors as forming a permanent acupuncture stimulus. The objective of this one-year double-blind, randomised, controlled trial was to investigate the effect of gold implantation at five acupuncture points in humans with knee OA on knee pain, stiffness and function as assessed by the patients as well as knee rating and function as assessed by an orthopaedic surgeon. Moreover, the time until a possible effect commences should be estimated, and it was to be examined whether the gold implants migrate. The study was carried out in a general practice in Holte, Denmark, from 1997 to 1998. After an appeal on TV, 102 patients volunteered. For inclusion in the trial they had to fulfil the following criteria: 1. age 18–80 years; 2. clinically diagnosed and radiologically verified knee OA; 3. pain and stiffness from knee OA for over a year. “Exclusion criteria were: previous knee trauma (OA following previous meniscectomy however was included); other rheumatic conditions such as rheumatoid arthritis or fibromyalgia; pronounced hip OA; severe somatic or mental illnesses; dementia; alcohol or drug abuse; pregnancy; anticoagulant treatment; corticosteroid treatment during the last 3 months; allergy to chlorhexidine or local anaesthetics.” 43 patients were suitable. They were assigned to a gold and a sham implantation group by random numbers (from Ciba-Geigy tables) by the Research Director of the Research Unit for General Practice, and the numbers were given to the main investigator (KN) one by one directly before randomisation of each patient. One patient had to be excluded one week after the gold implantation due to fibromyalgia. During the first month two other patients withdrew in order to have a knee joint prosthesis inserted. 40 patients thus remained for further analysis. The protocol was approved by the ethics commission of the district of Copenhagen. All patients signed a declaration of informed consent. At their first consultation, the original 43 patients were treated with conventional acupuncture at five points around the knee (Heding, Xiyan, St. 35, Gb. 33, Lr. 8) which affect arthritic knees according to Traditional Chinese Medicine (TCM). The immediate effect was assessed subjectively by the patients’ ability to walk on stairs. Two months later, the patients were randomised, and they were treated by the main investigator (KN) by implantation in one or both knees. The patients were unable to view the treatment on account of a screen. The five points mentioned were determined by acupuncture and locally anaesthetised with lidocaine-noradrenaline 1%. At each point a hypodermic 16-G needle was inserted and the tip positioned to the depth of the De-Qi sensation. The needle remained untouched for 4 minutes in order to make sure that it was placed outside the knee joint. In the case of patients with gold implantation, three cylindrical 24-carat gold beads of 1 mm x 2.5 mm and 35 mg were implanted through the needle at each point. A stylet was introduced and removed together with the needle. Directly after the procedure the knees of all patients were X-rayed in order to verify the location of the implants, if present. In a third consultation one week later, the patients were investigated for acute adverse effects. The main investigator next saw the patients 12 months later when the randomisation ceased for the patient. For evaluation the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was used. Before and 1, 3, 6, 9 and 12 months after the treatment the patients assessed pain (0–10 points), stiffness (0–8) and function (0–68) (lower number = milder symptoms) using the WOMAC questionnaire, and filled in another questionnaire about the use of analgesics. Furthermore, the same orthopaedist investigated the patients 1 month before and 6 and 12 months after the treatment using the Knee Society Clinical Rating System. A knee score rates the knee joint itself (0–100), a knee function score (0–100) rates the patient’s ability to walk and climb stairs (higher number = milder symptoms). Patients and orthopaedist were blind in relation to the treatment, and the completed questionnaires were evaluated only after the end of the study. The same radiologist assessed the X-ray images that had been made 2 months before as well as on the day of the treatment and 12 months later. The patients were not able to see the images. The severity of the knee OA was assessed by an ad-hoc score: 1/2/3/4 = no/some/moderate/severe bone attrition: joint space > 3 mm/< 3 mm/almost obliterated/obliterated. The results were to be analysed statistically. Since the only comparable studies were from veterinary medicine, there were no standards as to the sample size. Presuming a positive effect, the authors estimated that they would need 15 patients per group in order to detect a 2-point difference (SD = 2) in the WOMAC pain score with 80% power and 95% confidence. Since the results were the temporal development of the five predefined variables, a General Linear Mixed Model was applied to them, whereby the explanatory variables were treatment, time and their interaction. A separate level was modelled for every point in time. As a test for the significance of the differences between the treatments an F-test with null hypothesis was used, where all parameters with a fixed effect containing the treatment indicator of the patients are set at zero. The difference between the modelled initial value and the examination result after 12 months was evaluated as the overall change in a group. A Kruskal-Wallice test was used to gauge the difference of the 12-month results of both groups, independently of the development over the preceding months. The software PROC MIXED (SAS version 9.0) was used for statistical analysis. The nominal level for statistical significance was P < 0.05 (two-sided). During the study six patients were examined in various ways and partly treated (arthroscopy, removal of a Baker cyst and similar), but remained in the evaluation. The temporal development of the scores for pain, stiffness and function (from the WOMAC questionnaire) was depicted as an average over all 40 patients. Over the 12 months the pain score in the sham and the gold implantation groups dropped from 8.5 to 6.5 and from 8.0 to 4.5 [i.e. by about a half], respectively, while the stiffness score dropped from 4 (in both groups) to 3.5 and 2.5, respectively. The function score remained at 27 in the sham implantation group, while it dropped from 24.5 to 13.5 in the gold implantation group [i.e. by about a half, too]. When restricting the evaluation to the 32 patients who had responded to the initial acupuncture, the results were even more pronounced. [A diagramme for these 32 patients is not given in the paper.]
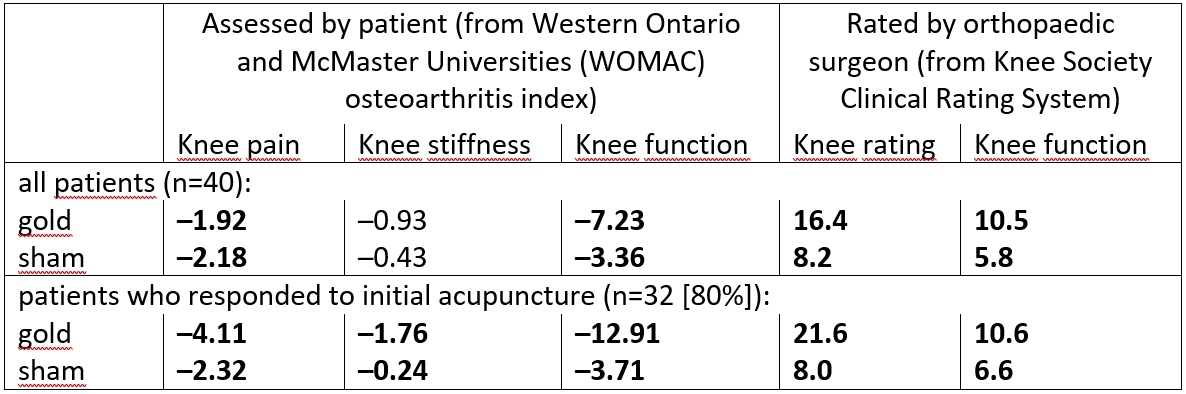
The effect of the gold implantation reached its maximum after 3 months, with no clear trend towards a further decrease or increase. The gold beads did not migrate, no patients had infections, nor did they experience rejection or discomfort. The treatment was tolerated well. Differences in the use of analgesics compared to the beginning could not be determined with certainty due to the low numbers, at least at the end of the study there did not seem to be more gold patients than sham ones using analgesics. At the end, 11 of 19 patients in the gold and 9 of 18 patients in the sham implantation group thought that they had obtained gold implants. The following differences between the modelled numbers at the beginning and after 12 months are given:
Especially when focussing on the 32 patients, most of these differences show clearly the effect of the gold implantation. According to the P values determined and the previously set target of P < 0.05, the authors, however, only consider the patient scores of stiffness and function as statistically significant [This is not likely to bother the patients.] Concluding, the authors point out that the patients’ knee OA was relatively mild and that it needs to be clarified whether the findings could be extended to patients with more severe knee OA. The results indicate that a possible effect of the gold implantation lasts for at least a year, but there are no long-term results available. The local anaesthesia and needle pricks produce a very strong acupuncture stimulus which could have reduced the observed relative effect of the gold implants. The TCM diagnosis of knee OA is very subtle, and the acupuncture should be individualised and use both local and distal acupuncture points. So it could be that the predefined points in the study were not optimal for all patients. The efficacy of manual acupuncture in the case of knee OA has been reported in three randomised, controlled trials and in several minor studies. This could explain some of the results of the sham implantation in the present study as owing to the needle pricks. 24-carat gold is non-toxic. The gold implants do not prevent the later insertion of a knee-joint prothesis. The procedure of gold implantation has to be done with precision and requires extensive experience with acupuncture. In some cases, it may be advantageous to implant gold more than once, since strong pain often masks weaker pain. The results of this pilot study suggest that gold implantation for patients with knee OA should be investigated in a larger trial.
|