News on joints from the health care system
Artificial joints can lead to metal deposits in the bones
According to new investigations, electrochemical reactions of the metals with their environment and also with each other can occur in artificial joints in which materials with different metal compounds are used. Metal ions are released into the tissue, which can attack the bone or lead to a thickening of the joint capsule and limited mobility. The authors suggest checking the metal concentration in the blood every five years. Source and further information: https://www.ndr.de/ratgeber/gesundheit/Kunstgelenke-koennen-zu-Metallablagerungen-im-Knochen-fuehren,huefte258.html 12 May 2019
Metal hip prostheses: poisoning by abrasion
Until recently, hip cap prostheses were regarded as a promising innovation, especially for younger and active patients. They were considered gentle on bones since the femoral head does not have to be removed. Instead, the cartilage layer is removed and “crowned”. Meanwhile, however, a drawback has arisen. The fairly large crowned surface of the ball permanently rubs against the large and fairly thin-walled socket. In this process apparently many prostheses show an increase in metal abrasion. Due to the abrasion products, extremely high levels of cobalt and chrome occurred in the blood of some of the persons concerned, many suffered from chronic poisoning. Typical consequences of such poisoning by metal abrasion include bone cysts, pseudo tumours and bone degradation. Furthermore, there is a slow build up of damage in the entire body, even as far as cardiac insufficiency. Source and further information: https://www.ndr.de/ratgeber/gesundheit/Metall-Hueftprothesen-Vergiftung-durch-Abrieb,huefte254.html
RTL shows how joint trouble can be alleviated by means of gold implantation on humans
The episode can be retrieved under this address: https://www.tvnow.de/rtl/der-naechste-bitte/hautarzt-dr-hans-georg-dauer-aus-koeln/player
Talk about gold implantation at the Medizinische Woche in Baden-Baden in 2018
On 3 November 2018, the surgeon Dr. Melanie Endrizzi from Düsseldorf gave a talk about “Gold implantation as an alternative method of pain treatment on joints with signs of arthrosis“ to a very interested audience. More deaths through resistant germs
Infants and elder people are especially at risk. In total, scientists estimate, the strain caused by antibiotic-resilient bacteria is as high as that caused by HIV/AIDS, influenza and tuberculosis taken together. According to the ECDC study, in total 671,689 infections due to antibiotic-resilient bacteria were registered within the European Economic Area in 2015. In this context, the authors warn of a “threat to modern health care”. They write about a severe burden, but also point to significant differences existing between the various EU countries. Read more on this at www.tagesschau.de/wissen/gesundheit/antibiotika-resistenz-103.html
Great success for gold implantation on humansRTL shows surgeon Dr. Melanie Endrizzi treating arthrosis complaints by means of gold implantation
The patient had been suffering from strong pain in her knee for almost 10 years. The filming location was Dr. Melanie Endrizzi’s practice in Düsseldorf. Those who want to know how the medical specialist for surgery finds pain points and inserts the small gold particles, 2 mm in size, near the joint, can obtain a good impression of it in this report. And best of all: after the first four weeks the patient depicts that she is now improving every day! The episode can be retrieved under this address: https://www.tvnow.de/rtl/der-naechste-bitte/hautarzt-dr-hans-georg-dauer-aus-koeln/player
Knee prostheses: patients frequently suffer from anterior knee pain
After the operation the structure of the knee joint has often changed. Various factors can then cause anterior knee pain (peripatellar pain syndrome). Here you learn more about its causes and about what helps in case of pain: www.ndr.de/ratgeber/verbraucher/Knieprothese-Was-bei-Schmerzen-hilft,kniegelenk132.html
Caution with hip surgery: danger of legs with different lengths
The larger the difference in the leg length, the higher the risk is of the hip tilting and of pain in the spinal column. Differences in length of more than one centimetre should be avoided. Researchers of the Fraunhofer Institute have developed a new method of measuring the leg length. In combination with a special hip prosthesis, it should be possible to adjust the leg length precisely. Read more here: www.ndr.de/ratgeber/gesundheit/Hueft-OP-Beinlaenge-praezise-messen,huefte234.html
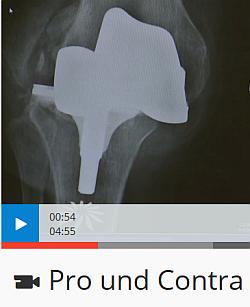
The pros and cons of knee surgery
In a film, the mdr radio (Mitteldeutscher Rundfunk) presents, amongst others, the results of a study conducted by physicians from Berlin and Munich. With most of the patients whose artificial joint had to be replaced due to problems, the prosthesis had been implanted for just six years only. It should actually last 15 years. In every fourth patient the artificial joint was not fitted stably, in 20 percent the angle was not correct. In every seventh patient the doctors detected an inflammation. The cause, as the study shows, is often due to the surgeons. Here you can watch the complete film: https://www.mdr.de/mediathek/mdr-videos/c/video-157814.html
Hip prosthesis. If there are no spare parts
Artificial joints should last for at least 20 years. Depending on the material, sooner or later surface wear or loosening occurs, and a replacement becomes necessary. In replacement surgery either the whole prosthesis or components such as the inlay, the socket or the hip head can be replaced. For some of those affected the complete prosthesis is exchanged because no spare parts are available for the inlay.
Source and further information:
Risk of anaesthesia – confused after surgery: lowering the risk
Typical symptoms include periods of disorientation, confusion, physical unrest, delusions and hallucinations. Many cases are a matter of temporary disorder without late consequences. However, about 40 percent of the persons concerned are so strongly limited in their mental capacity even a year after the incident that they depend on permanent care. Origin and further information:
Life-threatening infections possible owing to artificial joints
At the expense of the patientsIn Germany, in some regions people with back complaints are operated on up to 13 times more often than in other places. Their place of residence determines whether they come to hospital, are treated conservatively or undergo surgery. This is shown by the new study of the Bertelsmann-Stiftung (Bertelsmann foundation).
Furthermore, certain interventions occurred much more frequently in some regions than in others. The Bertelsmann study investigated the frequency of three selected back operations in all 402 districts (Kreise) und independent cities (kreisfreie Städte). It looked at how often spinal disc, stiffening and decompression operations were carried out. The conclusion of the study: “More and more patients are taken to hospital because of back pain – although this would often be avoidable.” Operating or not – obviously, this also depends on the habits of the doctors. “The decision for an operative intervention, however, must not be taken based on individual inclinations of the local doctors”, Eckhard Volbracht of the Bertelsmann Foundation urges. Instead, doctors should inform patients comprehensibly about the benefits and risks of treatment and decide together with the patient about the further approach independently of commercial interests.
Operating and cashing in – A crime novel about clinic dataSource: Das Erste In Germany, the residence alone often determines whether a patient is operated on or not. That’s the result of an extensive investigation and data analysis on behalf of the WDR (Westdeutscher Rundfunk).
But how do the clinics get so many patients? This also is revealed by the report through informants. The necessary patients are sent by registered physicians who have cooperation agreements with the clinics. Orthopaedists and neurosurgeons, for example, get a fixed price for certain operations from the clinics, in other cases a fixed percentage of the flat rate payment for every patient whom they bring to the clinic and operate on there. Suspicion of corruption raises its head. Another version are the so-called divided operation schedules, according to which two operations are performed successively that can actually be carried out together in one operation. The reason: this way the operations can be billed twice and at a higher price. This, too, happens at the expense of the patients: anaesthesia twice, being cut up twice – the double operation risk is obviously accepted in such cases. But the health insurance companies cannot afford to surveil all cases systematically – and nobody else as well so far. The film’s sad conclusion: “The winners are business-minded clinics and doctors, the losers are the patients.” You were able to watch the 44-minute film by Heike Hemschemeier until 19 June 2018 here.
Clinic germs cause 500,000 infections in Germany every yearAccording to a study published on 18 October 2016, in Europe, about 91,000 people die every year because they have caught an infection in a hospital. In Germany, too, the number of those affected is high. Petra Gastmeier, director of the Nationales Referenzzentrum zur Überwachung von Krankenhausinfektionen (national reference centre for the surveillance of hospital infections) at the Charité in Berlin, estimates that 500,000 patients annually become infected with hospital germs. Up to 15,000 patients die subsequently. Read the complete article here:
Scandalous competition with the wrong patientsIt must actually be in the interest of the health insurers to keep costs as low as possible. That’s why we expected considerable readiness on the part of the statutory (and of course also the private) health insurance companies to approve a cost-saving method such as gold implantation. But structures in the system apparently contradict it. To obtain as high a compensatory payment as possible from the so-called health fund, the statutory health insurance companies have systematically graded their members sicker than they actually are. This happens with the aid of doctors who categorise their patients and likewise make money from the severity of the illnesses, the executive director of the Techniker Krankenkasse, Jens Baas, says.1 It is a system out of which both doctors and health insurance companies make money. The worse the diagnosis, the more profitable it is.2 In the light of this, the interest in a diagnosis that “only” involves a gold implantation that is simply performed might thus be disappointingly low. Also the flat rate payments for joint operations in German hospitals contradict this (see our contribution of 1 September 2014: “Überflüssige Operationen: Nehmen Sie sich in Acht, wenn Ihr Arzt zu diesen Eingriffen rät“ (Superfluous operations: Be careful if your doctor recommends these operations)). Nonetheless, we keep on campaigning! In view of increasing antibiotic resilience and hospital infections, the health insurance companies will have to rethink. There are many more reasons for establishing this method which many people find so helpful.
Allergic to joint prostheses – what can be done?Allergies occur more and more often, also allergies to metal such as nickel, chrome or cobalt. If the person concerned needs a metal implant, for example an artificial knee or hip joint, this can have disastrous consequences. Due to the movement, ultrafine abrasion develops – not unusual with joint prostheses and normally no problem for the body, unless an allergy exists. Even patients who had no allergy beforehand can respond allergically to an implant. You find the complete article and a short film here:
Defective medical products: patients in dangerThey are supposed to help, but if defective they become a danger: medical products. Whether metal abrasion in the artificial hip joint, industrial silicone in breast implants, faulty electrodes in cardiac pacemakers or spinal disc prostheses, that become dislodged. The fatal thing is, the deficiencies are only recognised when the products have already done harm in the bodies of patients. Problems arise because the products had only been tested in the laboratory not on patients prior to being approved. To be approved, no clinical study is necessary, as in the case of pharmaceuticals, only material testing outside the body (CE sign). Here you can find the complete article and a short film:
Investigations owing to defective spinal disc prostheses?In the context of defective spinal disc prostheses, the Staatsanwaltschaft (public prosecutors) in Aurich is examining whether to initiate investigations at the Klinikum Leer. Recently it became known that defective spinal disc prostheses had been implanted in possibly more than 100 patients in this hospital. The British manufacturer Ranier had been delivering defective implants to Leer for years. 20 patients had already had to be operated on again because their spinal disc prostheses had become dislodged. As the manufacturer warns, the prostheses, clearly of inferior quality, would not grow on, in nearly every fifth case they would “wander around”. Here you can read the complete article:
Artificial hip joints often inadequately testedNovel artificial hip joints are allowed to be implanted into patients without clinical studies. In some cases, the little tested prostheses can lead to side effects. The report was on TV on 7 September 2015 in the programme Markt. You can watch it here:
29 Oct. 2014 Germans take too many antibiotics
to 15,000 people die from infections in hospital The new antibiotics report of the health insurance company DAK Gesundheit attests to the dramatic consequences of the frequent application of antibiotics in Germany. Especially in hospitals, resistant bacteria threaten the patients’ health. The analysis of the DAK hospital data shows that so-called hospital germs are being detected in more and more patients. Out of one million insured persons treated in hospitals in 2013, almost 20,000 carried a resistant germ in them. In 2010, it was only about 15,000 insured. This corresponds to an increase of almost one third. Throughout Germany and across all health insurers, 7,500 to 15,000 patients die annually from infections which arise in the course of hospital treatment.
Scandal: new knee and hip implants worse than old onesMore than 200,000 Germans get a hip or knee joint prosthesis every year. Generally, the complex surgery becomes necessary when the joint is affected by arthrosis. Those who rely on innovative products here are not well-advised, however. This is shown by a study of scientists from the Netherlands and the USA published in the British Medical Journal (BMJ). The researchers have analysed the data of patients with implants from 118 studies. This involved about 15,000 implants and about 13,000 people. The result: The scientists were not able to establish advantages of the new implants versus the proven ones. On the contrary, it has been shown that particularly the new technologies have made corrective surgery necessary. Summary from: Focus online Ratgeber of 11 September 2014
Superfluous operations: be careful if your doctor recommends these interventionsIn hardly any other country is there so much cutting, sawing, replacing and sewing up again as in Germany. This is shown by an international comparison of the Organisation for Economic Cooperation and Development (OECD). Some of these operations are superfluous, states the documentary filmmaker Meike Hemschemeier in her book “Vorsicht Operation” (Beware of surgery). Hemschemeier criticises amongst other things that hip and knee joint prostheses flush extreme amounts of money into the hospitals’ coffers. “As a result, patients are operated on again and again when, for instance, a physiotherapy could do the job as well”, says the author. (Remark of the Ackermann Team: or a gold implantation!) The Institut für angewandte Qualitätsförderung und Forschung im Gesundheitswesen (aQua) (institute for applied quality support and research in the health care system) has investigated how many of the hip and knee joint operations were medically justified. In 4.8 percent the surgery was not justified. This means, in one year doctors implanted an artificial hip or replaced it in almost 9,000 patients, although the surgery was unnecessary according to the aQua criteria. The institute investigated not only the hip but also the knee joint operations. Here, in one year 5,552 persons were operated on without it being medically justified. Other investigations reveal that many back operations bring little benefit in the long run. Moreover, they are carried out too often, as the number of the interventions shows. 735,000 spinal columns are operated on by surgeons every year, ten years ago there were half as many. The reason for this: Since 2003, the health insurers pay case rates for the medical effort. Several health insurance companies confirm that since the introduction of the case rates, especially the number of those operations for which the hospitals pay particularly well has gone through the roof. * Meike Hemschemeier: Vorsicht Operation! Wie wir zu Kranken gemacht werden und was wir dagegen tun können. 14,99 Euro, Pantheon. Summary from: Focus online Ratgeber of 1 September 2015
Botched job with artificial joints: what’s to be done?According to the latest statistics of the health insurance companies’ medical services, there were about 3,700 confirmed medical malpractices last year – but the dark figure is probably much higher. The Federal Ministry of Health assumes 40,000 to 170,000 instances. About 70 percent of the accusations of malpractice are directed at hospitals, 30 percent at registered doctors. Most of the examined medical malpractices occur after orthopaedic surgery, particularly in the case of implantations of hip and knee joint prostheses. You can read the complete article here:
|











 In Germany, people with back complaints have been admitted to hospital more and more frequently in recent years. Also, the number of spinal operations has started to increase strongly. From 2007 to 2015 it went up by 71 percent from 452,000 to 772,000.
In Germany, people with back complaints have been admitted to hospital more and more frequently in recent years. Also, the number of spinal operations has started to increase strongly. From 2007 to 2015 it went up by 71 percent from 452,000 to 772,000.








